Best practices for medical missions: 27 different guidelines, still lingering questions
May 16, 2018 |
Gone (we hope) are the days of North American volunteers parachuting into developing countries, distributing medicine, and then disappearing for good only days later. Below is the summary of an new academic article by Judith Lasker and colleagues on best practices for medical missions. Lasker is the author of Hoping to Help. And like Medical Service Trip, she is part of a movement to improve the quality of short-term global health projects now operating in dozens of developing countries abroad.
What’s wrong with short-term medical missions?
Critics lament the creation of dependency, lack of continuity of services, inadequate follow up, and discordance with local needs as strikes against the short-term medical mission model. But those things are almost impossible to do unless NGOs and volunteers have already devalued and excluded local providers. So: definitely don’t do that.
Other criticisms of global health experiences include the frequent lack of cultural aptitude (okay, sometimes accurate) and the charge of neocolonialism (which I see as an unfair slur). I’ve previously discussed how my mixed feelings on volunteer scope of practice and clinician credentialing have evolved.
Meanwhile, a limited body of research indicates that the real value of volunteers to host clinicians lies in partnership and communication with culturally competent visitors. All the better if they can bring necessary skills with them, and be open to reciprocal learning.

What they did, and what we did
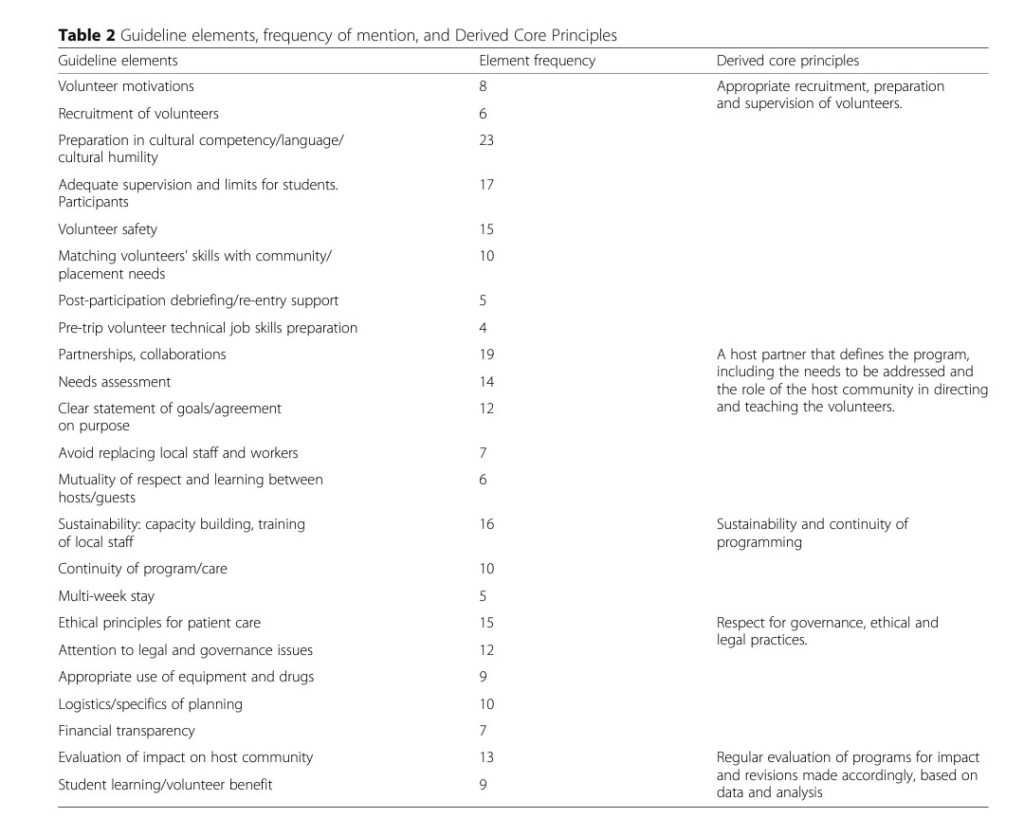
Lasker and colleagues found 27 sets of best practices for medical missions, mostly written by medical faculty and health practitioners. Only four had co-authors from host countries. Furthermore, NGOs were barely visible in the creation of these guidelines. It’s more evidence that some key voices are being shut out from the dialogue on the ethics of volunteering.
In comparison, our study asked a panel of academics, program administrators, and medical mission volunteers to review 30 host community oriented potential best practices. The discussion that followed ended with consensus on 18 of them, which now form our STAT best practices audit for NGOs and volunteers (which you can use right now to rate any of the 360 NGOs in our database). How do our elements relate to those in Lasker’s review?
In her study, Lasker identified 23 best practices for medical missions, volunteers, organizers, and host communities. Three were volunteer centred (volunteer safety, motivations, and learning), rather than host community oriented – and therefore not a part of our assessment. That left twenty to compare.
There are clearly best practices for medical missions that everyone agrees on
Eleven elements closely resembled items in our STAT inventory:
1. Preparation in cultural competence
2. Partnership and collaboration
3. Scope of practice and supervision of students
4. Capacity building by training of local staf
5. Volunteer recruitment
6. Post-participation debriefing
7. Pretrip job skills preparation
8. Avoid replacing local staff
9. Program continuity
10. Financial transparency
11. Logistics and planning
Similarly, the suggestion to Match skills with placement needs lines up roughly, but not exactly, with our suggestion that NGOs have an appropriate volunteer screening process. Meanwhile, three additional items were on our initial list of elements, but were ultimately rejected by our stakeholder panel.
1. Legal and governance
2. Needs assessment
3. Statement of goals/purpose
Two items (mutuality of respect and learning, and multi-week stay) were mentioned by a small minority of the guidelines. They both seem like good ideas, although the first is too subjective to be actionable.

The controversial items
Few would dispute the importance of the items below. It’s their execution that makes them stubbornly difficult to assess objectively.
1. Appropriate equipment/drug use
2. Evaluation of impact
3. Ethical principles for patient care
Nearly everyone agrees that evaluating program impact is critical – but how do we measure this, particularly for short-term medical missions delivering primary care? Our belief at Medical Service Trip, for example, is that impact and quality of care are measured through their proxies: adequate medical records and adherence to evidence based guidelines. Likewise, does the use of expired medications by short-term medical missions constitute expediency (after all, the vast majority of drugs do not lose their potency) or “dumping” unusable medications on the poor?
Until we adequately answer these questions, insisting on poorly defined criteria might set an impossible standard for NGOs – standards upon which reasonable people can disagree.
Register
Sign up for free to flag trips of interest and email organizations directly through our directory.
Comments
0 comments